What are medical billing codes?
Medical billing codes are shorthand for the healthcare industry. They are strings of letters and numbers assigned to every treatment, procedure, doctor’s visit, or medication you receive. When your insurance company receives a bill with these codes on them, they immediately know what they are being billed for and how much they will pay.
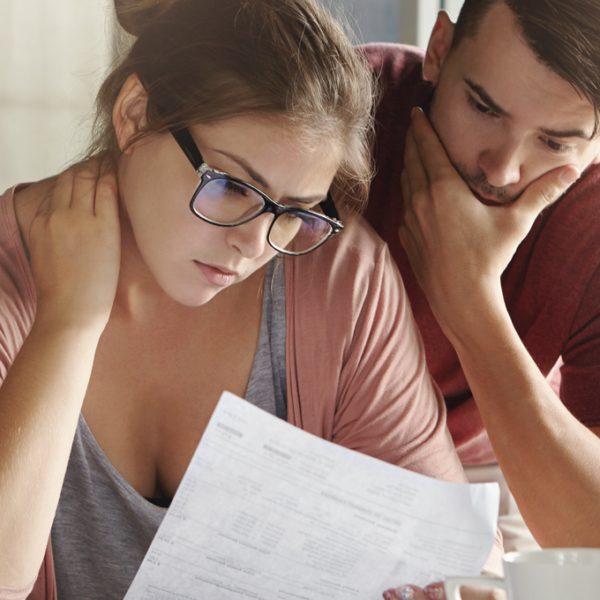
But the medical bills of the 21st century are complex and often difficult for regular people to interpret. While they create a universal “language” for anything medical-related, the truth is without proper training, you likely won’t be able to pick up any bill to see what you’re being charged for.
Understanding these codes goes a long way in ensuring you aren’t being overbilled or a victim of medical identity theft. But how can you protect yourself if you aren’t sure how to read them? That’s a big part of the reason why we created HealthLock—we help our members avoid the confusion of medical coding by automatically reviewing every bill as soon as you receive it.
To better understand how we do that, let’s take a high-level look at the world of medical coding.
What do medical codes cover?

Medical coding creates a uniform language that healthcare providers and insurance companies across the To better understand how we do that, let’s take a high-level look at the world of medical coding.
Medical coding creates a uniform language that healthcare providers and insurance companies across the country can read and understand. For example, if you receive treatment while on vacation in Hawaii, your doctor back home will be able to review the codes on your records and see exactly what happened, allowing a seamless transition of care.
The medical codes you see on your bills and explanations of benefits encompass things like:
- The diagnosis a patient receives
- Doctor’s visits
- Any tests the patient undergoes
- Prescriptions
- Equipment used
- Treatments, including medical devices
Providing each service and treatment a patient receives with a specific code makes it easy for a health insurance company to immediately decipher what it is being charged for. From there, they can determine how much they’ll pay vs. how much you will pay.
How many different types of medical codes are there?
There are several different medical codes in existence, but the three most frequently used are:
- International Classification of Diseases (ICD): The codes in the ICD tell your insurance company if you’ve been diagnosed with a fever or if you’ve broken a bone. The codes contained in the ICD relate to illnesses, injuries, and death. They are periodically updated to include new information. Depending on which version of the ICD code a doctor is working with, they may range from 14,000-68,000 entries.
- Current Procedural Terminology (CPT): These codes indicate what procedures you undergo in a healthcare facility, like surgery or a lab test. They are updated annually by the American Medical Association (AMA) and include categories representing the medical field (such as anesthesia or radiology).
- Healthcare Common Procedure Coding System (HCPCS): These codes tell your insurance company whether you’re receiving allergy medication or orthotic inserts. Like the two coding systems above, HCPCS includes numerous sub-categories and modifications to help craft an accurate diagnosis or bill.
How is medical coding misused?

There’s no question that medical coding has helped us build a stronger, more uniform level of healthcare. But while these codes can be helpful, their complexity makes it easy for medical fraud to occur. It only takes one switched number or letter to change the code, indicating an entirely different treatment, procedure, or diagnosis.
Because health insurance companies depend on these codes to determine reimbursement, an incorrect entry can lead to a claim being denied, and payment for that claim will fall solely on you. This is called overbilling, and while it is often accidental, it can also be used by healthcare providers trying to squeeze more profit out of their patients.
It’s estimated that American families are overcharged at least $1,687 per year. A large amount of that money might remain in the pockets of regular people if they understood the way coding operated and could identify incorrect codes.
That’s where HealthLock comes in. Using advanced AI technology, we monitor your healthcare bills to ensure the codes your healthcare providers are using line up with the services, treatments, and diagnoses you received. If we detect signs of overbilling or fraud through inaccurate medical codes, we can even help you get your money back.
You don’t have to become a medical coder to make sure the information on your medical bills is correct. Let HealthLock take care of that for you—you can leave your security and peace of mind to us.